Patients taking GLP-1 medications for weight loss and blood sugar control reported some surprisingly interesting changes in their habits. They found it easier to resist cravings and cut back on addictive behaviors, particularly around food.
“Anecdotally, people with food addiction who find GLP-1s helpful in this regard talk about how the medication turns down the volume of ‘food noise’ in the brain, by which they mean the constant thoughts and cravings for certain types of food,”
– Anna Lembke, MD, professor of psychiatry and behavioral sciences at Stanford Medicine
These patient reports prompted researchers to take a closer look at what was happening in the brain.
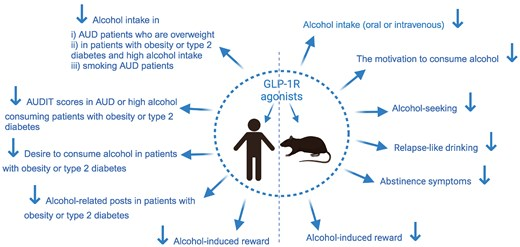
Studies reveal that GLP-1 medications act on the brain’s reward and dopamine systems, the same neural circuitry that drives addiction.
This discovery has led to multiple studies exploring whether these drugs could help treat not just food-related compulsions, but a broad spectrum of addictive behaviors.
Scientists are now investigating GLP-1’s potential effectiveness against alcohol use disorder, opioid addiction, and nicotine dependence. Some are even exploring whether the medications could help with behavioral addictions like gambling, compulsive sexual behavior, and compulsive shopping.
The interest has grown intense enough that some doctors have begun prescribing GLP-1 medications off-label, meaning for uses not yet approved by regulators like the FDA, to treat various addictions.
Much of the research remains in early stages, but a picture is emerging of what these drugs can and can’t do in addiction treatment. The findings so far suggest both remarkable promise and significant limitations.
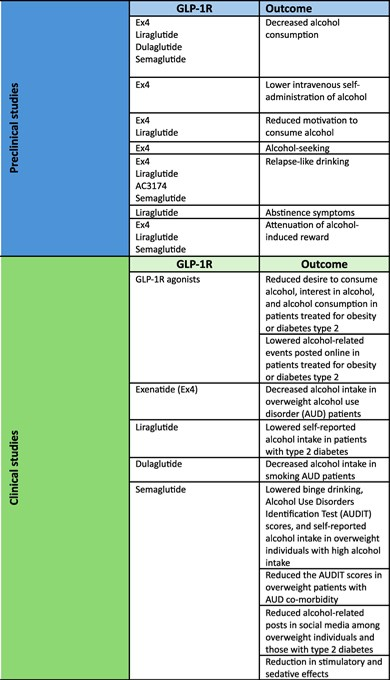
Here’s what studies have found so far:

Could a diabetes drug help treat alcohol addiction? Research suggests yes.
Scientists are uncovering an unexpected potential for semaglutide, the active ingredient in popular weight-loss medications like Ozempic and Wegovy. They are looking at it as a treatment for alcohol use disorder.
The drug, which belongs to GLP-1 medications, appears to dramatically reduce both alcohol cravings and drinking behavior. That’s drawing attention from addiction specialists.
Clinical trials
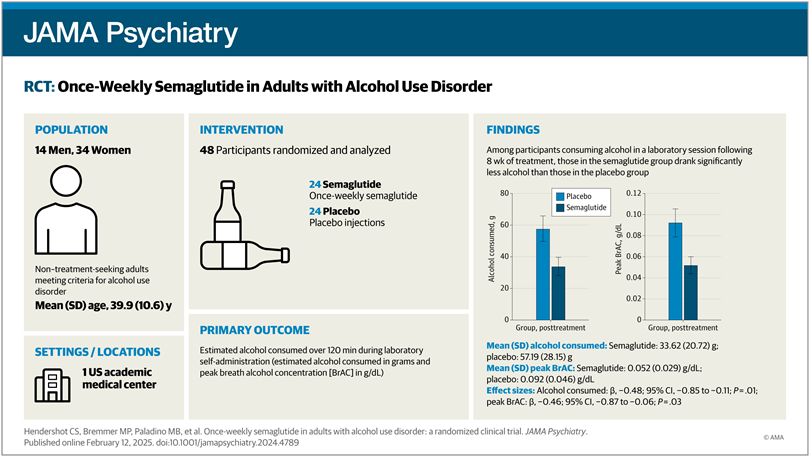
UNC (University of North Carolina) School of Medicine conducted a phase 2 clinical trial to examine semaglutide’s effects on people with alcohol use disorder. Researchers documented striking results in this trial.
Participants reduced their alcohol consumption by 48 percent, meaning they drank less than half as much as before. Their cravings for alcohol fell by 41 percent, and episodes of heavy drinking also declined.
The study also revealed an additional, unexpected benefit: Participants who smoked cigarettes also cut back on their tobacco use during the trial.
Real-world evidence from Sweden
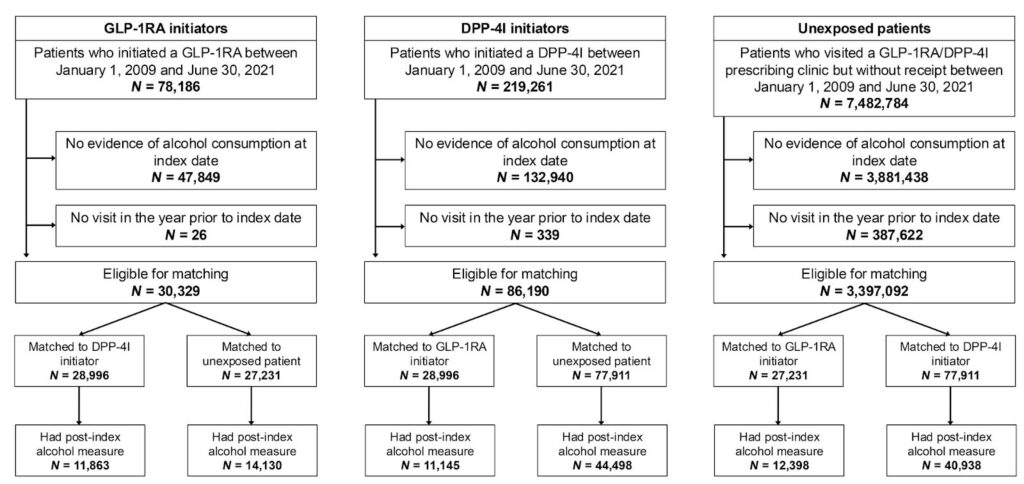
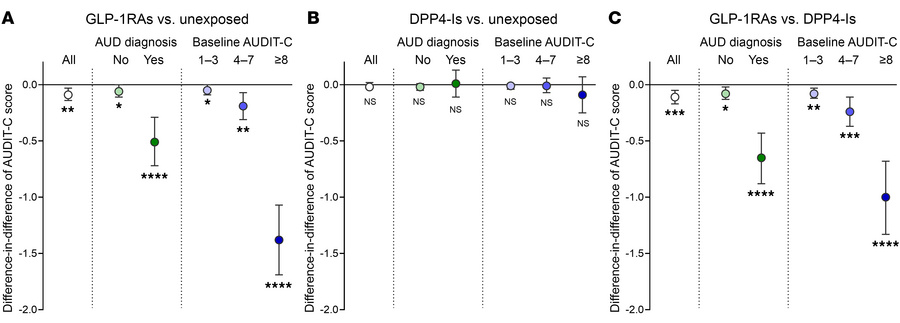
The clinical findings are supported by a thorough analysis of Swedish health records spanning nearly two decades. Researchers examined data from 227,866 people between 2006 and 2023 and found that those taking semaglutide experienced 36 percent fewer alcohol-related hospital visits compared to those not taking the medication.
Another GLP-1 class drug, liraglutide, showed similar but slightly less pronounced effects, reducing alcohol-related hospitalizations by 28 percent.
Confirmation through blood tests
Laboratory evidence supports these population-level trends. Blood tests from studies of exenatide, another GLP-1 medication, showed that the drug reduced alcohol consumption compared to placebo.
The effects became measurable after 20 weeks of treatment, providing objective biochemical confirmation of what patients reported experiencing.
GLP-1 medicines can help overcome nicotine addiction without side effects (like weight gain)
Clinical studies show that GLP-1 medicines reduce the urge to smoke and the rewarding feeling people get from nicotine. These medications block the pleasant dopamine rush that nicotine normally creates in the brain’s reward center. They also reduce the uncomfortable side effects of quitting, like cravings, withdrawal symptoms, and overeating. This changes how the brain responds to nicotine, making smoking less enjoyable and easier to resist.
What’s interesting is that these effects last even after stopping the medicine.
This is proven in trials looking at long-term results of GLP-1 medicines on nicotine addiction. People who participated in these trials avoided relapsing into smoking at 24 weeks and 52 weeks. The study also showed that these medicines prevented the weight gain side effect of quitting smoking.
We analyzed these insights on emerging GLP-1 uses and research using SLATE. This research tool can help R&D teams find, organize, and simplify data with one simple query, like:
What are the emerging therapeutic applications of GLP-1 receptor agonists in addiction medicine?

GLP-1 hacks the brain’s reward system and makes ditching opioids easy
Combining GLP-1 medications with other drugs offers better results in fighting opioid addiction. GEP12, a new drug that combines GLP-1, Y1, and Y2 receptor targets, is being studied in animals. It reduced the fentanyl intake and their desire for the drug, without affecting their eating habits or causing negative side effects.
This worked in the same way as for alcohol addiction: by blocking the dopamine surge that fentanyl causes.
Another drug, Liraglutide, has shown promise in preventing heroin cravings in rats. It reduced the drug-seeking behavior caused by stress, environmental cues, or exposure to the drug itself.
Will GLP-1 and its combinations work similarly on humans with opioid or heroin addictions?
Researchers are finding answers to this and similar questions through an ongoing clinical trial involving 40 adults with opioid addiction. This trial looks at how liraglutide affects cravings triggered by different situations. Advanced brain imaging techniques are helping them understand the results more clearly.
A few players are a step ahead of others and have already started filing patent applications.
One of these applications describes pairing GLP-1 medications with another type of drug that blocks orexin receptors (orexin-1 or orexin-2) in the brain for treating opioid addiction. As per claims, this will be especially effective in reducing cravings triggered by external cues or stress.
A new pathway to overcome cocaine addiction
In a pilot study, researchers tested exenatide, a GLP-1 medication, on three people with cocaine use disorder. The participants received weekly 2-milligram injections for six weeks, and the results were encouraging.
All three patients completed the full course of treatment and attended every scheduled session. They reported satisfaction with the outcomes, and researchers observed no serious or unexpected side effects. While the study was small, it provided crucial early evidence that the approach merits further investigation.
Real-world experiences mirror these clinical findings. Susan Akin, a 41-year-old patient at Caron Treatment Centers in Florida, began receiving Zepbound, another GLP-1 medication, for cocaine and alcohol addiction earlier this year.
For Akin, the weekly injections have been transformative. She can now visit trigger-filled environments like gas stations without craving beer or encounter sugar without wanting to contact her cocaine dealer.
“I know when I’m due for my shot because I get a little antsy or irritable, or just kind of off,” she said. “But it has changed my life.”
– Susan Akin
The cravings haven’t vanished entirely, but they’ve become manageable. A quieting of what she describes as the chaos that once dominated her thoughts.
What makes GLP-1 drugs particularly intriguing is that they appear to work through a mechanism distinct from traditional addiction treatments.
Researchers discovered that the body’s natural GLP-1 system activates specific brain cells called GABA neurons (gamma-aminobutyric acid) in a region called the ventral tegmental area, or VTA. This brain structure sits at the heart of our reward system, the circuitry that governs how we experience pleasure and motivation from food, drugs, and other rewarding stimuli.
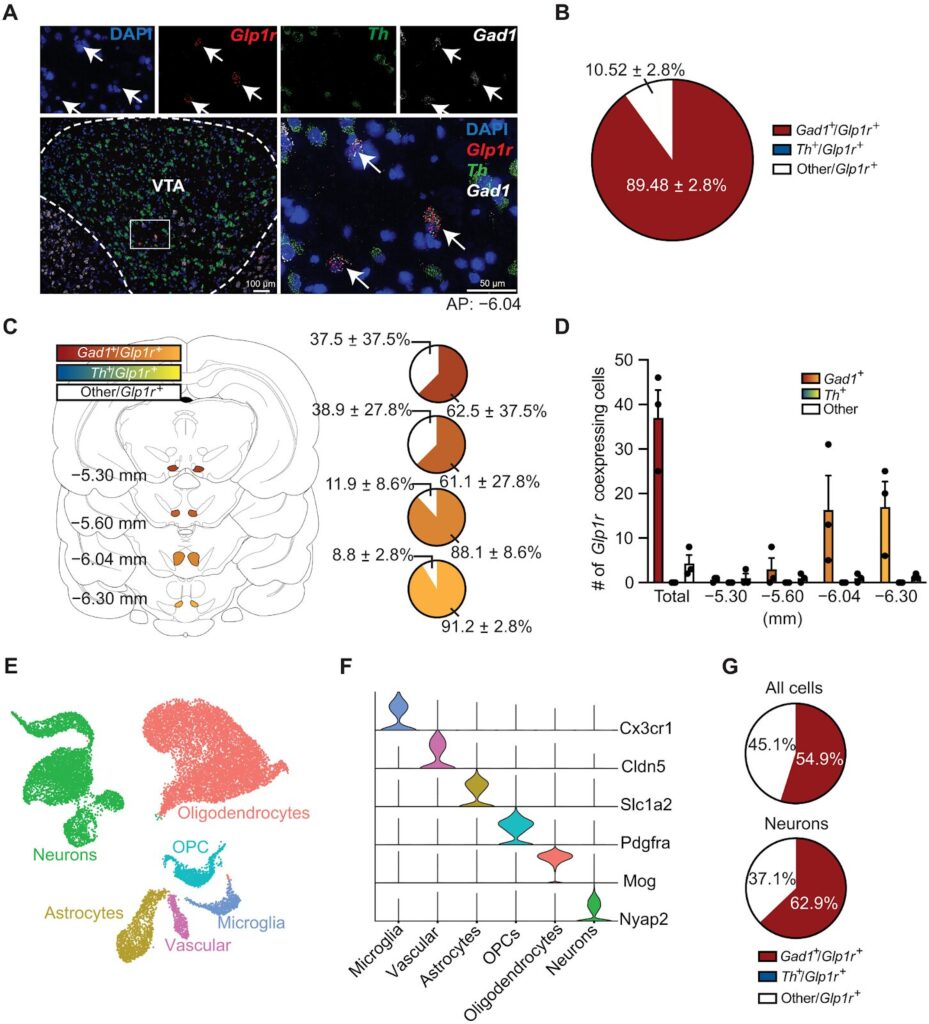
GABA neurons act as the brain’s brake system that helps control neural activity. When GLP-1 hormones stimulate these neurons, they essentially “calm” certain parts of the brain, reducing both cravings and the urge to use cocaine. This represents a fundamentally new type of addiction treatment, one that sidesteps the dopamine-focused methods that have dominated the field.
Mapping the brain’s response
Researchers went further, pinpointing exactly which brain regions GLP-1 affects in combating addiction. For instance, injecting GLP-1 directly into specific areas, including the lateral septum, ventral hippocampus, and nucleus accumbens, reduces alcohol consumption.
These targeted experiments suggest that these particular brain regions play critical roles in how GLP-1 medications help fight addiction. It can help researchers draw a roadmap for developing even more effective GLP-1-based treatments for addiction medicine.
Addiction treatment centers are already prescribing GLP-1 medicines to patients
While clinical trials continue, some major addiction treatment facilities, or at least one, aren’t waiting for the final verdict on GLP-1 medications.
Caron Treatment Centers in Pennsylvania has started using GLP-1 medicines as part of its standard addiction treatments. These bold experiments are offering an early glimpse of how the medications might work in real-world clinical settings.
From research to practice
At Caron, patients now receive GLP-1 medications, administered either once daily or once weekly, alongside established therapies such as cognitive-behavioral therapy and traditional 12-step programs.
Early observations from the center suggest the combination may be yielding benefits: Patients appear to be staying in treatment longer, and many report reduced cravings.
Such integrations also reflect a growing willingness among some clinicians to explore novel approaches to addiction treatment.
A physician-led experiment
Steven Klein, an addiction medicine specialist at Caron, is leading a pilot program that represents one of the most extensive real-world tests of GLP-1 drugs for addiction to date. Klein has prescribed these medications to more than 130 patients across facilities in Pennsylvania and South Florida.
His patient population includes people diagnosed with alcohol use disorder as well as some who use stimulants. This expands the potential applications beyond the alcohol-focused research that has dominated studies so far.
What about side effects?
One concern with any new treatment approach is tolerability, particularly for a population already dealing with complex health challenges. So far, the safety profile appears reassuring.
Across various trials, the most common side effects have been mild gastrointestinal issues: nausea, vomiting, or diarrhea. The same complaints are familiar to millions who have taken these drugs for diabetes or weight loss.
In addiction treatment settings specifically, patients have generally tolerated the medications well, and clinicians have reported no unexpected or severe adverse effects.
Where the research stands and where it’s heading
As the FDA has not approved GLP-1 drugs for addiction treatment, they are still not covered by insurance companies. Most patients are “piggybacking” these medications through their insurance by receiving them under FDA-approved uses, or by paying out of pocket with manufacturer discounts.
Pharmaceutical manufacturers are beginning to acknowledge the addiction treatment potential of their blockbuster GLP-1 products. Eli Lilly, which makes Zepbound, has stated it is considering clinical trials to assess the drug as a treatment for substance use disorders, including alcohol and tobacco dependence.
These companies (Eli Lilly and Novo Nordisk) also announced plans to lower direct-to-consumer prices as part of a deal with the Trump administration.
These moves may improve accessibility for patients currently using these medications off-label for addiction.
Trials underway
The research pipeline is beginning to fill. Several Phase 2 trials are currently testing semaglutide for alcohol use disorder, including studies registered as NCT05895643 and NCT05520775.
Interest among addiction treatment centers in incorporating these metabolic drugs into their therapeutic programs continues to grow. The early clinical adoption suggests that some practitioners believe the potential benefits outweigh the risks.
What’s still needed
Despite the momentum, significant gaps remain. Researchers emphasize that large-scale, randomized trials are essential to confirm how effective these drugs truly are for addiction treatment.
Scientists are also working to identify specific biological markers, genetic or metabolic traits, that could help determine which patients will benefit most from these treatments. This personalized medicine approach could make the difference between success and failure for individual patients.
Looking further ahead, researchers are focusing on developing GLP-1 drugs specifically engineered to better penetrate the central nervous system.
These next-generation medications would be designed from the ground up to target addiction pathways, rather than being repurposed from diabetes and obesity treatments.
Conclusion
GLP-1 drugs are offering a new way of thinking about addiction treatment, using a metabolic approach. They already show strong evidence for helping with alcohol use disorder and have promising potential for treating nicotine, opioid, and cocaine addiction. This creates options for future product development and therapeutic strategies for the pharma, nutrition, and medical industries.
Therefore, tracking ongoing research, competitor moves, and new opportunities is important for companies to become early movers and gain a competitive advantage.
Slate can help you with this tracking. It is made explicitly for researchers and development teams to help find relevant, high-quality results by eliminating noise.












