In May 2025, Dexcom issued a Class 1 recall for its G6, G7, ONE, and ONE+ receivers due to a speaker malfunction. The failure of the speaker to produce an alert for dangerously high or low blood sugar levels was identified as a critical patient safety issue. This problem led to the ~56 cases of seizures, loss of consciousness, vomiting, and hypoglycemic or hyperglycemic symptoms in consumers.
These types of technical issues raise questions about the reliability of existing Continuous Glucose Monitors (CGMs).
A recent review also shows that CGM technologies have predictable performance degradation issues. Their accuracy drifts within 72 hours of insertion, and they need frequent recalibration. Additionally, the sensor behaves differently when the temperature changes or it comes into contact with moisture from sweat. This environmental sensitivity makes CGM devices unreliable during critical moments, such as when patients are exercising, ill, or stressed, when blood sugar levels are most likely to fluctuate.
Healthcare giants like Roche, Abbott, and Medtronic, and startups like Percusense and Dual AI, understand the importance of upgrading CGMs to improve patient care and gain a competitive edge. They are investing in AI integration, automated algorithms, and advanced sensor technologies to make glucose monitoring preventive, easy, and affordable.
Source: Slate Dashboard
Here are a few notable patented innovations in glucose monitoring devices:
These insights are part of our detailed report on Glucose Monitoring innovations. Fill out the form to receive your copy of this report:
1. A CGM that can monitor heart rate, oxygen, lactate, and not just glucose
Current CGM devices only focus on glucose and do not track any other factors that can affect blood sugar and insulin needs. For example, existing continuous glucose monitors do not consider everyday physiological states like exercise, meals, sleep, and stress that can affect blood sugar and insulin needs. This causes reactive and poor long-term glucose control, which can lead to risks like hypoglycemia.
Percusense, a US medtech startup, proposed a solution to fill this gap with a patent-pending CGM device that has multiple sensors to measure changes in other biomarkers continuously, along with glucose.
By analyzing data of changes in other biomarker(s) like lactate, oxygen, reactive oxygen species (ROS), or ketones, the system can detect if the person is sleeping, eating, stressed, or exercising. Its adaptive algorithm continuously learns the user’s unique physiological patterns. Based on these patterns, it can predict the changes in blood sugar and prevent risks like hypoglycaemia.
This continuous glucose monitor can be integrated with artificial pancreas (AP) and automated insulin delivery (AID) systems. It can help in real-time automatic insulin delivery based on the physiological state and needs of the body.
This device can also be connected wirelessly to a phone, smart watch, or cloud system to send data and analyze trends.
PercuSense compared its continuous multi-analyte (glucose-lactate) sensor against Medtronic’s Guardian 3 CGM in a clinical study. In results, the new glucose sensor worked almost as well as Medtronic’s Guardian 3, with accuracy improving after a few days of use. Although the lactate sensor was less precise, it still clearly indicated rises in lactate level during exercise.
This device is yet to launch. Once commercialized, it can reduce the burden (data integration, cost) of using multiple devices for patients and the healthcare industry. Patients will not have to wear multiple sensors like a heart monitor and Continuous Ketone Monitor (CKM), along with CGM, to track these biomarkers and complete care. Glucose monitoring will come one step closer to becoming closed-loop.
2. AI-Powered CGM that predicts food-induced blood sugar spikes and recommends prevention strategies
Current glucose monitoring systems often fall short in predicting how specific foods impact a person’s blood sugar levels, which can lead to dangerous spikes, especially for individuals with diabetes or pre-diabetes. This problem arises because traditional methods, such as carb counting and post-meal testing, do not offer real-time insights into food-induced glucose fluctuations, resulting in missed opportunities to prevent spikes.
Dula AI, a Florida-based startup, proposes an innovative solution with an AI-powered health system that combines continuous glucose monitoring (CGM) with personalized food and activity tracking.
This continuous glucose monitoring system captures real-time glucose data from the user and, via an AI server, predicts and alerts the user to potential food-induced glucose spikes. It works by linking the glucose data with other contextual information, such as food intake (logged via photos or manual entries) and physical activity, which are recorded by the mobile app. If a spike is detected or anticipated, the system alerts the user. It provides personalized recommendations, such as adjustments to food intake or activity, to help maintain glucose levels within a safe range. The system reduces the stress and uncertainty associated with managing glucose levels.
The system’s key advantages include real-time, AI-driven alerts and recommendations, which offer a proactive approach to glucose management as opposed to reactive systems currently on the market.
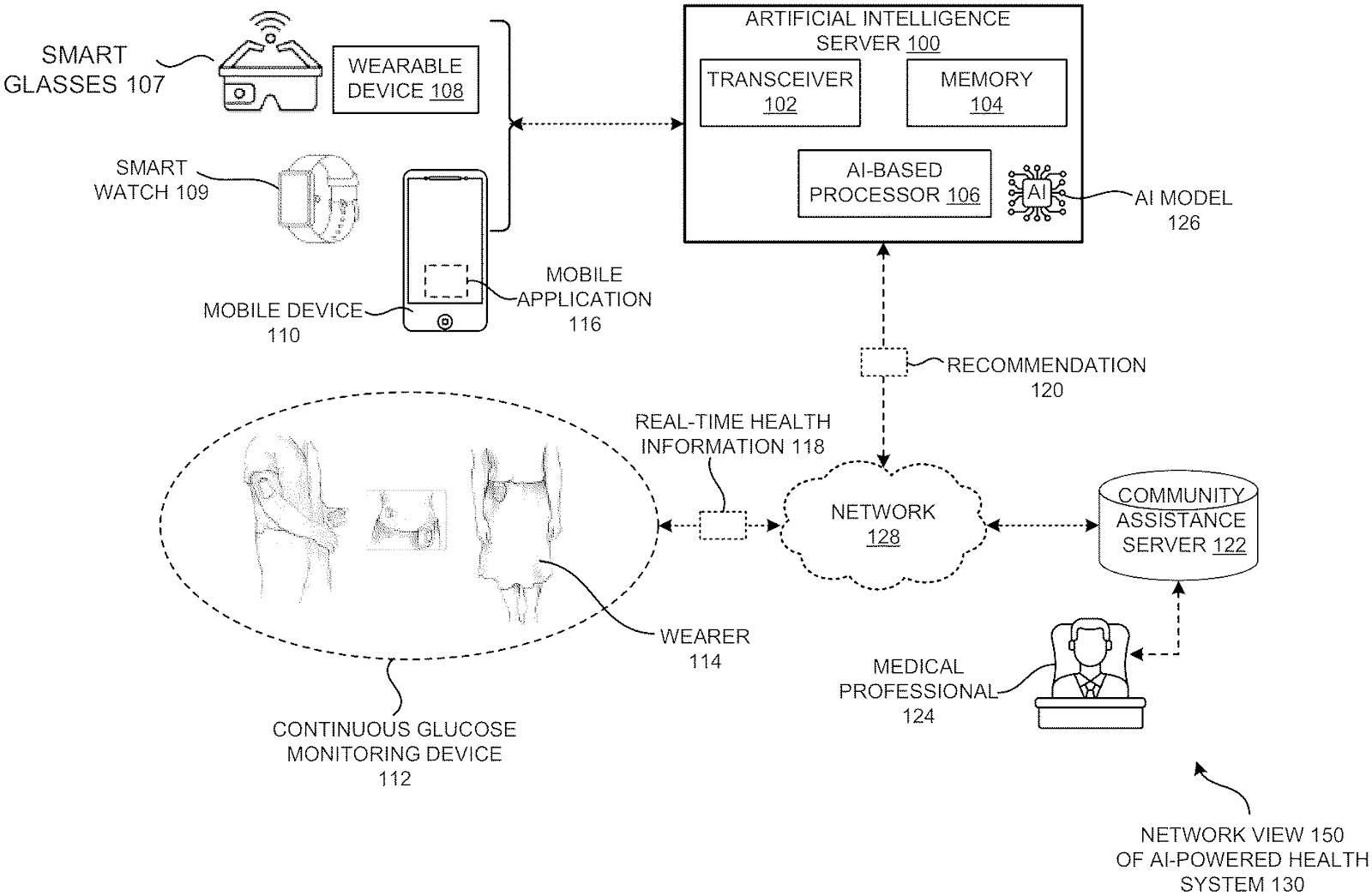
The technology also integrates seamlessly with wearables, offering a user-friendly and scalable solution. It is still patent-pending and not yet commercially available. If it is successfully brought to market, it could significantly improve glucose management for diabetes patients.
3. This CGM filters out corrupted signals for more accurate glucose readings
Blood glucose readings captured by current CGMs are corrupted by external factors, such as meals, exercise, sleep, or other usual disruptions like the user’s behavior or environmental changes. This reduces the quality of data and can result in missed opportunities for early detection of blood glucose abnormalities. It can also lead to late intervention in managing diabetes or preventing its onset.
Continuous glucose monitors are also inconvenient to wear, still invasive, and sometimes costly.
Huawei came up with an innovative wearable device that uses photoplethysmography (PPG) signals to monitor blood glucose levels non-invasively. The device collects PPG data from the user over time. This data is filtered using AI algorithms to filter out low-quality or corrupted blood glucose readings that are affected by external factors.
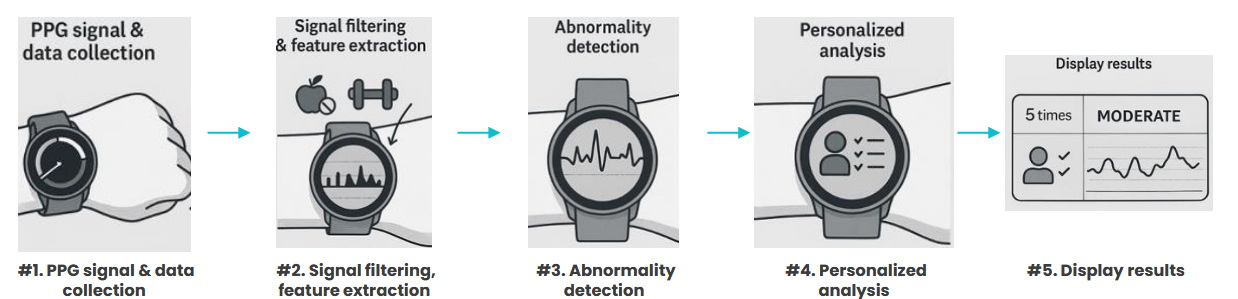
This filtration ensures the device only analyzes relevant, clean signals and shows more accurate glucose information for the individual.
The system breaks the PPG signals into smaller time samples to identity abnormalities or out of the normal range glucose levels. A graphical interface on the wearable device also displays the frequency of blood glucose abnormalities and provides a visual representation of risk levels over time.
Its analysis model uses the basic information of the wearer, like age, health status, and other factors, to provide personalized glucose risk predictions. This approach helps users better understand their glucose status and potential risks for developing conditions like diabetes.
Its personalized nature also makes this system more clinically relevant, as it can adapt to the unique needs of each user. This level of customization enhances the overall accuracy and effectiveness of the glucose monitoring.
Additionally, the use of a wearable format such as a smartwatch increases the scalability of this technology, making it easy for consumers to use it regularly.
Huawei has already launched this technology in its Watch 4 series in China. This is the first commercially available non-invasive high blood sugar assessment smartwatch. This marks the first step in bringing this innovative technology to the mass market.
What’s Next
Diabetes and related complications and their costs are rising continuously. They are still consuming nearly 20% of the Gross Domestic Product (GDP). Making blood sugar-related healthcare technologies preventive, simple, and affordable is important for the healthcare industry to control this cost. At the same time, meeting the growing demands for personalized and non-invasive solutions is necessary for companies to stay competitive and profitable.
Apart from AI algorithms and wearable technologies, companies are exploring the integration of biosensors into wearables. They are combining electrochemical and optical sensors to improve accuracy and comfort. Some startups are also focused on non-invasive sensors that measure glucose from sweat and tears.
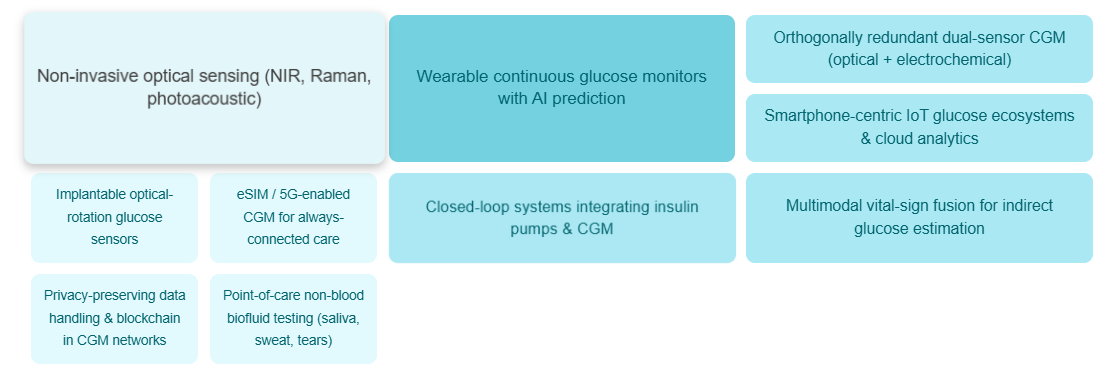
Innovations are happening in all areas related to continuous glucose monitoring technologies, starting from devices and ecosystems, sensors, and microneedles to AI algorithms.
Tracking these innovations while constantly refining the existing products is a crucial but overwhelming task for your R&D team.
That’s where GreyB comes in. Our experts can closely track new developments in the industry to identify potential collaboration and acquisition opportunities suitable for you. Fill out the form to know: